Diagnostic and Therapeutic Hysteroscopy
What is Hysteroscopy?
The invention of the hysteroscope brought a major advancement to gynecology.
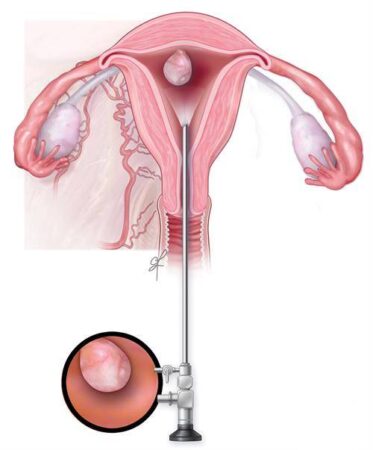
A hysteroscope is a thin telescope-like device that is inserted through the vagina and cervix to visualize:
- The cervix and vaginal canal
- The endocervical canal
- The endometrial cavity
- The openings of the fallopian tubes
The hysteroscope is connected to a monitor, allowing the surgeon and their team to clearly observe the uterine cavity and perform diagnostic or therapeutic interventions at the same time.
Hysteroscopy can therefore serve both diagnostic and therapeutic purposes.
Indications for Hysteroscopy:
Hysteroscopy may be recommended in cases such as:
- Abnormal uterine bleeding before or after menopause
- Thickened endometrium or suspected endometrial polyps
- Submucosal fibroids or selected intramural fibroids
- Intrauterine adhesions (Asherman’s syndrome)
- Congenital uterine anomalies (e.g., septate uterus)
- Retained intrauterine devices (IUD) or foreign bodies
- Retained products of conception after miscarriage or delivery
- Permanent sterilization
- Certain endocervical lesions
- Recurrent implantation failure during infertility treatment
- Endometrial ablation (removal of the uterine lining)
- Evaluation of the cervical canal when embryo transfer catheters cannot pass
- Patients unable to undergo more invasive surgeries
Contraindications:
Hysteroscopy is not performed in:
- Ongoing intrauterine pregnancy
- Active pelvic infections (e.g., genital herpes)
- Known cervical or endometrial cancers
- Severe cardiovascular disease
Advantages of Hysteroscopy Over Other Diagnostic Methods:
Compared to pelvic ultrasound, sonohysterography, or hysterosalpingography, hysteroscopy provides direct visualization of the uterine cavity. In addition, many pathologies can be treated during the same procedure.
However, hysteroscopy cannot evaluate conditions within the myometrium (e.g., adenomyosis) or fallopian tube pathology. In such cases, combining hysteroscopy with laparoscopy is recommended.
Preoperative Assessment:
- Complete medical history
- Full pelvic examination with special attention to uterine size, mobility, and tubal status
- Pregnancy test
- Cervical culture and treatment in case of cervicitis
The patient must be informed of possible risks and sign an informed consent. These include:
- Early termination of the procedure due to excess fluid absorption
- Risk of uterine perforation
- Potential conversion to laparoscopy or laparotomy if vascular or visceral injury is suspected
Patient Preparation:
- Scheduling the procedure:
- Premenopausal women: best performed shortly after menstruation (within the first week). For therapeutic hysteroscopy, medications may be prescribed to thin the endometrium beforehand.
- Postmenopausal women: procedure can be performed at any time.
- Cervical preparation:
- Cervical dilation is often required, especially in postmenopausal women or those with a history of cervical stenosis or surgery.
- Misoprostol may be prescribed orally or vaginally the night before or the morning of surgery, depending on the physician’s instructions.
Other preoperative considerations:
- Use of hormonal medication if prescribed
- Use of cervical dilators as directed
- Treating any vaginal or cervical infections prior to surgery
- Avoiding vaginal douches, tampons, or creams 24 hours before surgery
- Showering and shaving the genital and abdominal area
- Discontinuing Aspirin and Warfarin 72 hours prior, and Heparin 24 hours prior (if applicable)
- Fasting for at least 8 hours before surgery
- Removing jewelry, watches, makeup, nail polish, glasses, dentures, hearing aids, lenses, or prosthetic nails before entering the operating room
- Emptying the bladder immediately before surgery
How Hysteroscopy is Performed?
- The patient is positioned in the lithotomy position (legs in stirrups).
- The external genitalia, vagina, and cervix are disinfected.
- Anesthesia is administered (diagnostic hysteroscopies are often performed under sedation, while therapeutic ones usually require general anesthesia).
- A speculum is inserted, and the cervix is dilated with special instruments to allow the passage of the hysteroscope.
- To improve visualization, the uterine cavity is distended with saline solution or, if electrocautery is needed, with a different distension medium.
- The surgeon can either look directly through the hysteroscope or use video monitoring on a large screen.
- If necessary, miniature surgical instruments are introduced through the hysteroscope to remove polyps, fibroids, or adhesions.
- Since 1–3% of uterine lesions may be missed during hysteroscopy, an endometrial biopsy is usually performed, especially in women with unexplained persistent bleeding.
- After the procedure, the patient is monitored in recovery before returning to the ward.
Discharge After Hysteroscopy
- Most patients are discharged the same day.
Possible Complications
Although rare, complications may include:
- Uterine perforation (0.12%)
- Fluid overload
- Internal bleeding
- Bladder, bowel, or cervical injury
- Endometritis (uterine infection)
- Embolism
- Urinary tract infection
- Intrauterine adhesions (Asherman’s syndrome)
Contact your doctor immediately if you experience:
- Fever
- Severe abdominal pain
- Heavy vaginal bleeding
- Foul-smelling vaginal discharge
- Difficulty urinating
- Shortness of breath
Common Postoperative Symptoms
- Mild abdominal cramping
- Light vaginal bleeding
- Vaginal discomfort
- Nausea (due to anesthesia)
- Dry or sore throat (from anesthesia)
Postoperative Care
- Take pain relievers (e.g., ibuprofen) every 8 hours if needed
- Complete the prescribed antibiotic course
- Resume light daily activities after 24 hours
- Climb stairs and do light household work as tolerated
- Driving is safe after 3 days
- Showering is allowed the day after surgery
- Sexual activity may resume 5 days after surgery, or once vaginal bleeding stops
- Exercise can usually be restarted in 5–10 days
- Swimming is permitted after 7 days
- Avoid heavy lifting for 2 weeks
- Return for follow-up and pathology results within 7–10 days
- Hormonal therapy (estrogen and progesterone) may be prescribed to promote endometrial healing; it is essential to follow the doctor’s instructions and not stop medication on your own
- In some cases, a temporary intrauterine device (IUD) or catheter may be placed to prevent adhesions; your doctor will remove it at the appropriate time
- The first menstrual cycle after hysteroscopy may be heavier, longer, or irregular compared to normal