Chorionic Villus Sampling (CVS)
Chorionic Villus Sampling (CVS)
What is CVS?
Chorionic Villus Sampling (CVS) is an invasive diagnostic test performed during pregnancy to assess the health of the fetus. It involves collecting and analyzing chorionic villi, which are small finger-like projections from the placenta. Since these villi share the same genetic material as the fetus, their evaluation provides important genetic information.
During CVS, a sample of these villi is collected and sent to a genetics laboratory for testing.
When is CVS performed?
- CVS is typically carried out in the late first trimester, most commonly between 11 and 13 weeks of pregnancy.
- It is usually delayed until after 11 weeks, since most spontaneous miscarriages occur before this time, and performing CVS too early may increase the risk of fetal limb abnormalities.
- Although CVS can be performed after 14 weeks, amniocentesis is generally preferred beyond 15 weeks.
Who should consider CVS?
CVS may be recommended in the following cases:
- Women aged 35 years or older at the time of delivery.
- Abnormal results in prenatal screening tests (e.g., cell-free DNA screening).
- Detection of structural abnormalities in the first-trimester ultrasound.
- Parents who previously had a child with a chromosomal abnormality or genetic disorder.
- Parents who are carriers of chromosomal structural abnormalities.
- Parents who are carriers of single-gene disorders.
- Couples who are both carriers of the same autosomal recessive condition.
- Mothers who are carriers of X-linked genetic disorders, where determining the sex of the fetus is especially important.
Who should not undergo CVS?
CVS is not recommended in:
- Mothers with alloimmunization.
- Pregnancies with an IUD in place that has not been removed.
- Mothers infected with HIV, Hepatitis B, or Hepatitis C, as there is an increased risk of transmitting infection to the fetus.
In such cases, Amniocentesis is often a safer alternative.
CVS vs. Amniocentesis
Advantages of CVS:
- Provides results 4–6 weeks earlier than amniocentesis.
- Preferred for diagnosing certain metabolic and genetic conditions, such as PKU or thalassemia.
Disadvantages of CVS:
- Slightly higher risk of miscarriage compared to amniocentesis.
- Results may be less definitive, with a greater chance of detecting confined placental mosaicism.
- Cannot detect neural tube defects, unlike amniocentesis.
Preparing for CVS
Before the procedure, the following steps are recommended:
- Treat any vaginal or cervical infection.
- Coordinate with the genetics laboratory and obtain the sample collection kit.
- Sign the informed consent form.
- Undergo an ultrasound (the day before or same day) to assess fetal number, heartbeat, and structural anomalies.
- Shower and shave the genital and abdominal area.
- Fast for at least 8 hours.
- Remove jewelry, watches, hair accessories, makeup, and nail polish before entering the operating room.
- Remove glasses, dentures, hearing aids, contact lenses, and nail prosthetics.
- Stop taking Aspirin at least 72 hours before and Heparin 24 hours before (if applicable).
- Have a semi-full bladder (drink a glass of liquid about an hour before the procedure).
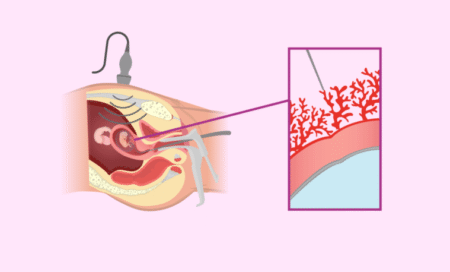
How CVS is performed
CVS can be performed in two ways:
- Transabdominal method:
- The patient lies on her back while the location of the placenta is determined using abdominal ultrasound.
- The lower abdomen is disinfected, and after local anesthesia or sedation, a biopsy needle is guided into the placenta under ultrasound.
- A small tissue sample is taken and sent in a culture medium to the genetics lab.
Advantages:
- Lower risk of miscarriage, bleeding, and infection.
- Higher chance of obtaining a clean, uncontaminated sample.
- Transcervical method:
- After disinfecting the genital area and inserting a speculum, ultrasound is used to identify the placenta’s position.
- Following short anesthesia, a thin catheter is inserted through the cervix and guided into the placenta.
- A syringe containing special culture medium is attached, and chorionic villi are aspirated.
- The sample is sent to the genetics lab for testing.
Advantages:
- Generally less discomfort for the patient.
- Lower risk of maternal–fetal bleeding.
- Reduced risk of bowel injury.
The choice of method depends on the location of the placenta and the position of the uterus and fetus, as determined by the physician.
Results are usually available within 1–2 weeks. In some cases, if results are inconclusive or the sample is insufficient, a repeat CVS or an amniocentesis may be required.
Risks and Possible Complications of CVS
- Miscarriage: occurs in approximately 7 per 1,000 procedures.
- False results: extremely rare (false-negative rate ~0.03%).
- Sampling failure: less than 1% of cases.
- Mosaicism: sometimes the placental tissue differs from the fetus’s genetic makeup.
- Fetal limb injury: more likely if CVS is performed before 10 weeks.
- Bleeding or spotting: common but usually mild; heavy bleeding must be reported.
- Infection: rare, usually from contamination of instruments with vaginal or skin flora.
- Transmission of maternal infections (HIV, hepatitis, CMV, toxoplasmosis) is possible.
- Maternal–fetal hemorrhage: can lead to isoimmunization; Rh-negative mothers must receive anti-D (RhoGAM) injection after CVS.
- Premature rupture of membranes (PROM): rare, but fluid leakage should be reported.
- Some studies suggest a slightly higher incidence of placental abruption and preeclampsia in women who undergo CVS.
Post-procedure Care
- Progesterone injection as prescribed.
- RhoGAM injection for Rh-negative mothers with Rh-positive partners.
- Antibiotics if recommended by the physician.
- Pain relievers if needed.
For the first 24 hours:
- Rest in bed (relative rest).
- Drink plenty of fluids.
For 3–4 days after CVS:
- Avoid lifting heavy objects.
- Avoid strenuous activity.
- Avoid sexual intercourse.
If CVS was performed transcervically:
- Do not use tampons.
- Avoid baths and swimming pools.
- Showering is allowed the same day.
Common Post-CVS Symptoms
- Light spotting or brown discharge.
- Mild bruising or abdominal discomfort (after transabdominal CVS).
- Mild cramping for 24–48 hours.
Warning Signs – When to Call Your Doctor
Seek medical attention immediately if you experience:
- Heavy vaginal bleeding.
- Foul-smelling discharge.
- Clear fluid leakage from the vagina or abdomen.
- Severe pelvic or uterine cramping.
- Fever or chills.
- Severe abdominal pain.