Amniocentesis
Amniocentesis
Amniocentesis is a diagnostic test performed to evaluate the health of the fetus before birth.
The test involves analyzing the amniotic fluid, which surrounds the fetus inside the uterus. Amniotic fluid contains fetal urine, secretions, and shed cells from the fetus. By examining this fluid, physicians can assess the baby’s health and development.
When is Amniocentesis Performed?
Amniocentesis may be recommended for:
- Prenatal genetic testing (the most common reason)
- Detection of neural tube defects
- Assessment of fetal lung maturity
- Evaluation of fetal infections
- Measurement of fetal blood and platelets to determine the severity of hemolytic anemia
- Diagnosis of fetal hemoglobinopathies
Sometimes, amniocentesis is performed for therapeutic purposes, such as draining excess amniotic fluid in cases of polyhydramnios.
Timing of Amniocentesis
- For genetic testing, amniocentesis can technically be done anytime after 11 weeks, but the recommended period is between 15–18 weeks of pregnancy.
- Performing the procedure before 15 weeks increases the risk of miscarriage and complications, such as inaccurate results, middle ear defects, and clubfoot. Therefore, it is not advised.
- After 18 weeks, the procedure is still possible, but if severe abnormalities are detected, terminating the pregnancy may be more complicated.
Turnaround Time for Results
The reporting time depends on the type of genetic testing performed:
- Full karyotype (complete chromosomal analysis): 7–14 days
- Limited chromosome analysis (chromosomes 13, 18, 21, X, and Y): 1–2 days
- Microdeletion/duplication analysis: 3–5 days
Preparations Before Amniocentesis
Before the procedure, patients should:
- Obtain a referral letter from their treating physician
- Register with a genetics laboratory and coordinate testing
- Collect the sample container from the genetics lab
- Complete and sign the informed consent form (by both partners)
- Stop taking Aspirin 72 hours before and Heparin 24 hours before the procedure (if prescribed)
- Undergo ultrasound to confirm fetal viability, placental location, fetal position, fetal measurements, and amniotic fluid assessment
- Shower and shave the abdominal area
- Fasting is not required
- Remove jewelry, watches, hair accessories, and personal items before entering the procedure room
- Avoid makeup, nail polish, dentures, contact lenses, hearing aids, or artificial nails
- Empty the bladder immediately before the procedure
How Amniocentesis is Performed
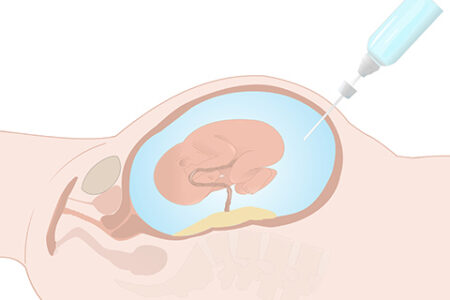
- The patient lies on a flat table. The abdomen is cleaned with an antiseptic solution and draped.
- Using continuous ultrasound guidance, the physician inserts a thin, long needle through the abdominal wall into the uterus, away from the placenta and fetus.
- A small amount of amniotic fluid is withdrawn into a syringe and sent to the genetics laboratory.
- A follow-up ultrasound is performed immediately afterward to check the fetal heartbeat and ensure fetal well-being.
Anesthesia:
- General anesthesia is not required. The patient remains awake.
- In anxious patients, or if sampling is needed from the lower uterus, local anesthesia may be given.
- Local anesthesia numbs only the skin entry site. Mild discomfort or cramping may still be felt when the needle passes through the uterine muscle.
Possible immediate side effects:
- Mild uterine cramps
- Light spotting
- Minor leakage of amniotic fluid through the vagina
Aftercare Following Amniocentesis
Medications:
- Progesterone injection, if prescribed
- Anti-D immunoglobulin (300 mcg) for Rh-negative mothers with Rh-positive partners
- Antibiotics, if prescribed
- Pain relievers, if needed
On the day of the procedure:
- You may eat and drink normally. Drink plenty of fluids (water or juice every 1–2 hours) to replace lost fluid and reduce cramping
- You may shower
- Avoid heavy activity; rest in bed (sitting or lying) for the remainder of the day
- Do not drive, exercise, lift heavy objects, take long walks, or have sexual intercourse
- Mild abdominal, pelvic, or back discomfort is common
- Light spotting may occur and last up to 2 days. Use only sanitary pads (not tampons)
The next day:
- If you feel well, you may return to work and resume daily activities
For 3 days (72 hours) after the procedure:
- Avoid strenuous physical activity or sports
- Avoid sexual intercourse
- Do not lift heavy objects
- Do not use bathtubs or swimming pools
- Avoid long-distance travel for 5–7 days
When to Contact Your Doctor
Seek immediate medical attention if you experience:
- Heavy leakage of amniotic fluid
- Heavy vaginal bleeding (heavier than a menstrual period)
- Fever or chills above 38°C
- Severe abdominal cramps
- Foul-smelling vaginal discharge
Risks and Complications
Amniocentesis is generally safe, but possible risks include:
- Premature rupture of membranes
- Direct injury to the fetus
- Maternal infection
- Miscarriage: Risk is about 0.2–0.3% when performed by an experienced specialist under ultrasound guidance. Most miscarriages occur within 4 weeks after the procedure.
Risk factors include: less experienced operator, repeated attempts, elevated maternal AFP, fetal anomalies, vaginal bleeding during pregnancy, or history of ≥3 miscarriages. - Transmission of maternal infections (e.g., Hepatitis, CMV, Toxoplasmosis, HIV): In such cases, alternative tests like cell-free DNA are preferred.
- Rarely, contamination by intestinal bacteria if the needle punctures the bowel, leading to infection, miscarriage, or septic shock
- Amnionitis (infection of amniotic fluid): very rare
- Leakage of amniotic fluid (usually resolves within 1 week and is replaced within ~3 weeks)
- Separation of the amnion from the chorion (rare; usually no impact on pregnancy outcome)
- Indirect fetal complications (respiratory or orthopedic issues), especially if the procedure is done before 15 weeks or if prolonged leakage occurs.
- Cell culture failure (~0.1%), requiring repeat sampling
- Mosaicism (0.1–0.2%), requiring fetal blood sampling and genetic consultation