Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection (ICSI)
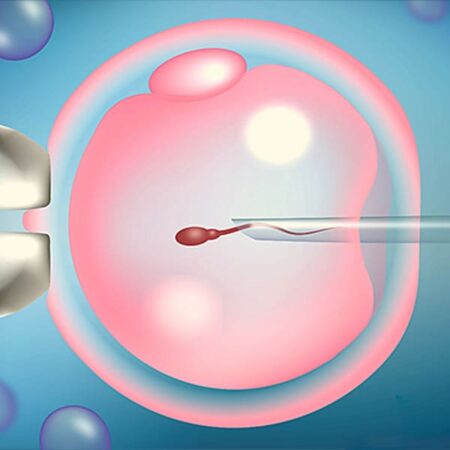
ICSI is a groundbreaking technique in the treatment of male factor infertility. In this procedure, an embryologist uses a high-powered microscope to distinguish healthy sperm from abnormal ones. A single immobilized sperm is then injected directly into the cytoplasm of a mature egg using an extremely fine needle.
ICSI is performed in approximately 30 – 40% of infertility cases due to male factors and is particularly beneficial in the following situations:
- 1 Low sperm count
- 2 Poor sperm motility
- 3 High percentage of abnormally shaped sperm
- 4 Obstruction in the epididymis or testicles preventing sperm release
- 5 Presence of anti-sperm antibodies
- 6 Prior vasectomy
- 7 Failed or poor fertilization in standard IVF
- 8 Retrograde ejaculation
ICSI Process: Step-by-Step
Step 1: Patient Education
Patients receive thorough education about the ICSI procedure, potential risks, benefits, and medication administration techniques. This may be done through brochures, the clinic’s website and social media, and consultation with medical staff.
Step 2: Ovarian Stimulation
The goal is to produce multiple mature eggs rather than just one. Strong ovulation-inducing medications are prescribed.
- The cycle typically begins with a baseline ultrasound on day 1 or 2 of menstruation. If normal, stimulation medications are started.
- Regular ultrasounds and blood tests are used to monitor follicular development.
- Once follicles reach maturity (typically 15–18 mm), an HCG injection is administered to trigger final maturation. Egg retrieval is scheduled approximately 36 hours later.
- In some cases, a GnRH agonist may be used instead of HCG to reduce the risk of complications.
Potential Side Effects
While the medications themselves are generally well tolerated, ovarian enlargement due to multiple developing follicles may cause bloating, abdominal discomfort, nausea, or vomiting.
Ovarian Hyperstimulation Syndrome (OHSS)
- A rare but serious complication caused by excessive ovarian response.
- Symptoms include severe abdominal pain, nausea, and risk of blood clots or fluid imbalance.
- Occurs in mild form in 2–6% of stimulated cycles, and in severe form in about 1%.
- Risk is higher with more than 20 mature follicles or elevated estradiol levels. It can be mitigated by cycle cancellation, using GnRH agonists instead of HCG, or performing IVM (in vitro maturation).
- Symptoms typically peak 3–5 days after egg retrieval. A decision to transfer or freeze embryos is made during this period.
Step 3: Egg and Sperm Retrieval
- Egg retrieval occurs 32–36 hours after HCG injection under light sedation and ultrasound guidance, using a thin needle via the vaginal route. no surgical incision is required.
- The male partner provides a sperm sample concurrently.
- In cases where no sperm is present in the ejaculate (azoospermia), surgical sperm extraction (TESE or Micro-TESE) may be performed beforehand, and frozen sperm is used on the day of egg retrieval.
Patients typically return home a few hours after the procedure but should avoid driving or working for 24 hours.
If a fresh embryo transfer is planned, progesterone supplementation (via suppository or injection) begins on the day of the egg retrieval or day after.
Possible Complications from Egg Retrieval
Rare but may include:
- Pelvic cramps
- Light vaginal bleeding
- Increased vaginal discharge
Persistent or severe symptoms should be reported to the physician.
Step 4: Fertilization (ICSI Procedure)
In the lab, a single sperm is injected into the egg under a microscope using a microneedle. Fertilization rates with ICSI range from 50 –70%.
Step 5: Embryo Transfer
- Performed 3–5 days after fertilization.
- One or two high-quality embryos are transferred into the uterus using a soft catheter, without anesthesia or pain.
- If conditions like poor endometrial receptivity or OHSS risk are present, embryos may be frozen and transferred in a later cycle.
- Studies show that frozen embryo transfers may offer higher pregnancy rates than fresh transfers. At Pooyesh Fertility Clinic, the majority of embryo transfers are frozen.
How Many Embryos Are Transferred?
The number depends on the woman’s age, embryo quality, previous pregnancy history, and risk of miscarriage.
- Women under 35 undergoing their first ICSI cycle are typically recommended a single embryo transfer.
- In cases of repeated failed cycles, two embryos may be transferred to increase success—this also raises the risk of twin pregnancy.
- Women over 40 often receive more embryos due to lower implantation potential.
PGT (Preimplantation Genetic Testing)
Couples who carry hereditary genetic disorders or mutations may opt for PGT to screen embryos before transfer. PGT can also be used for gender selection. However, this testing does not replace routine prenatal screening.
Pregnancy Testing After ICSI
- A β-HCG blood test is performed about two weeks after embryo transfer.
- A level below 5 indicates no pregnancy; a level above 10 suggests pregnancy, but the test must be repeated after 48 hours to confirm progression.
- Ideally, β-HCG levels double every 48 hours for the first 21 days.
- Inadequate rise or decline may indicate embryo loss or ectopic implantation.
Ultrasound Monitoring
- If β-HCG levels rise appropriately, the first ultrasound is done 3 – 4 weeks after embryo transfer.
- By 5 – 6 weeks gestation, the yolk sac (which nourishes the embryo early on) should be visible.
- The fetal heartbeat is typically detected at 6 to 6.5 weeks gestation.
Prenatal Care After ICSI
Routine prenatal care typically begins between 6 and 10 weeks of gestation.