Preimplantation Genetic Testing (PGT)
Preimplantation Genetic Testing (PGT)
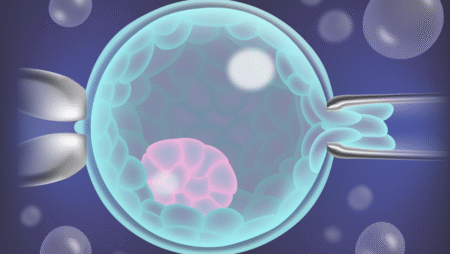
Preimplantation Genetic Testing (PGT) is performed through various methods, all of which are carried out following IVF or ICSI procedures.
The most common method of PGT also used at Pooyesh Fertility Clinic involves biopsy of blastocyst-stage embryos (day-5 embryos). Based on the genetic test results, selected embryos are frozen and later transferred to the uterus in subsequent frozen embryo transfer (FET) cycles.
PGT is performed for the following purposes:
- To detect chromosomal abnormalities (PGT-A):
Formerly known as Preimplantation Genetic Screening (PGS), this method examines embryos for abnormalities in chromosome number, even when both parents appear genetically healthy. Theoretically, avoiding the transfer of such embryos can reduce the risk of miscarriage and pregnancy loss, while increasing the chances of a successful, healthy pregnancy. - To detect single-gene disorders (PGT-M):
The aim is to achieve a pregnancy free of specific genetic disorders inherited from one or both parents. - To detect structural chromosomal abnormalities (PGT-SR):
This includes translocations, deletions, or duplications of chromosome segments. - For sex selection:
This may be done for medical reasons such as preventing the transmission of sex-linked genetic disorders like hemophilia or for non-medical reasons, such as parental preference for a specific gender.
Other indications for PGT include:
- 1 Advanced maternal age in patients seeking elective single embryo transfer
- 2 Improving pregnancy outcomes in IVF patients
- 3 Repeated IVF failure
- 4 Recurrent miscarriage
Safety of Embryo Biopsy
Blastocyst Biopsy (Day 5 Embryos):
Biopsy of blastocyst-stage embryos (day 5 embryos) has not been shown to negatively impact implantation rates or live birth rates compared to non-biopsied embryos.
Cleavage-Stage Biopsy (Day 3 Embryos):
Biopsying embryos on day 3 (which typically have 6 to 10 cells) may be associated with a reduced implantation rate.
Congenital Abnormalities
In cases involving preimplantation genetic testing (PGT), the rate of congenital abnormalities is not higher than that seen in standard IVF procedures. This means that embryo biopsy does not increase the risk of birth defects.
Congenital Abnormalities
In cases involving preimplantation genetic testing (PGT), the rate of congenital abnormalities is not higher than that seen in standard IVF procedures. This means that embryo biopsy does not increase the risk of birth defects.
Short-Term Neonatal Outcomes
Some studies have reported that certain complications are slightly more frequent in pregnancies achieved through PGT compared to other types of pregnancies. These include:
- Increased risk of pregnancy-induced hypertension
- Higher incidence of small-for-gestational-age (SGA) infants
- Increased rates of preterm birth
Childhood Development
Research has shown that children conceived via PGT who are between the ages of 5 and 6 years demonstrate normal development in terms of motor skills, psychological well-being, emotional health, and cognitive function comparable to peers conceived without PGT.
PGT Counseling
Couples considering PGT should receive counseling from a qualified specialist.
Key points to be covered during the consultation include:
- The patient must return to the clinic eight days after egg retrieval to receive the genetic results, chromosomal sex report (X and Y chromosomes) for each embryo, and the embryo cryopreservation card.
- The likelihood of obtaining an embryo with both the desired genetic profile and preferred sex is approximately 20%.
- Genetic testing costs are calculated per embryo and are the responsibility of the patient.
- The clinic is responsible for transferring biopsy samples to the genetic laboratory.
- To minimize error, all procedures are conducted in the presence of a second witness.
- The chance of pregnancy per transferred embryo ranges from 0% to 40%, depending on the woman’s age, and the quality of both eggs and sperm.
- There is about a 5% chance that the pregnancy outcome may not match the genetic test results.
Cycle Cancellation
Approximately 30% of PGT cycles are canceled due to the following reasons:
- Failure to develop good-quality blastocysts suitable for biopsy and freezing
(In 10% of cases, none of the embryos reach the blastocyst stage) - Inability of the genetic lab to provide a report due to technical issues.
In such cases, re-biopsy may be considered after consultation with the embryologist - Aneuploidy detected in biopsied embryos, such as abnormal sex chromosome compositions (e.g., XYY, YO, XO, XXX, XXY)
Requires follow-up consultation with the embryologist - Absence of embryos with the desired sex among those tested and frozen
PGT Results Are Not Definitive
It is important to note that PGT does not guarantee absolute accuracy. For all pregnancies resulting from PGT, confirmatory prenatal genetic testing is recommended via:
- Chorionic villus sampling (CVS) or
- Genetic amniocentesis
Of the two, genetic amniocentesis is generally preferred, as it more accurately reflects the chromosomal status of the fetus rather than the placenta.