Cervical Cerclage
Cervical Cerclage
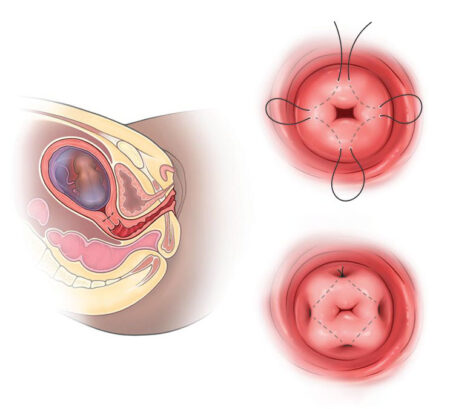
Cervical cerclage is a surgical procedure in which the cervix is stitched during pregnancy to reinforce its strength and prevent complications associated with cervical insufficiency.
Consequences of Cervical Insufficiency in Pregnancy
- Prolapse of the fetal membranes into the vagina
- Infection of the amniotic fluid (chorioamnionitis)
- Premature rupture of membranes (PROM)
- Preterm labor and delivery
- Pregnancy loss
In most cases, cerclage is performed via the vaginal route.
Candidates for Cervical Cerclage
Cerclage is recommended for pregnant women who:
- Have a history suggestive of cervical insufficiency in previous pregnancies
- Show cervical shortening on transvaginal ultrasound
- Have cervical dilation detected on vaginal examination
Contraindications for Cerclage
Cerclage should not be performed in cases of:
- Major fetal anomalies incompatible with life
- Intrauterine infection
- Premature rupture of membranes
- Miscarriage in progress
- Active uterine bleeding
- Placenta previa (though in selected cases, cerclage may still be considered)
- Protrusion of fetal membranes through the external cervical os
Timing of Cervical Cerclage
- 12–24 weeks of gestation (ideally before 18 weeks): The usual window for cerclage placement.
- Before 12 weeks: Not recommended, as genetic and structural screening of the fetus is not yet complete, and natural miscarriages due to chromosomal abnormalities may occur during the first trimester.
- 24–28 weeks: Controversial. Some specialists avoid cerclage after fetal viability (24 weeks), while others may proceed due to the high risk of fetal morbidity and mortality. Decisions are individualized and may include alternatives such as pessary placement.
- After 28 weeks: Rarely performed, since delivery after this gestational age generally has favorable outcomes.
Pre-Cerclage Evaluation
- Confirmation of gestational age and fetal cardiac activity
- Screening for chromosomal abnormalities
- Assessment and treatment of cervical and vaginal infections
- Screening for urinary tract infections
- Evaluation for signs of preterm labor, premature rupture of membranes, or placental abruption
Preoperative Preparation
- Treat vaginal or cervical infections before the procedure
- Shower and shave the genital area
- Fasting for at least 8 hours
- Remove jewelry, watches, hair accessories, cosmetics, nail polish, and prosthetics (dentures, hearing aids, contact lenses, etc.) before entering the operating room
- Empty bladder immediately before surgery
- Discontinue Aspirin 3 days prior and Heparin 1 day prior (if applicable)
- Avoid sexual intercourse for at least 1 week before the procedure
- Prophylactic antibiotics may be prescribed at the physician’s discretion
Surgical Technique
In the operating room, after disinfecting the vagina and cervix and administering light anesthesia, the cervix is grasped with forceps. A thick, non-absorbable suture is then placed in a purse-string fashion approximately 2 cm above the external os and securely tied.
Discharge After Surgery
- Cerclage is an outpatient procedure. The patient is discharged once anesthesia has worn off and normal movement and urination are restored.
- Fetal heart rate and amniotic fluid volume should be evaluated and documented before discharge.
Possible Complications
- Light vaginal spotting
- Uterine cramps
- Difficulty urinating (these usually resolve within a few days)
- Lower abdominal or back pain similar to labor pains
- Increased vaginal discharge
- Leakage of amniotic fluid, which may result in miscarriage
- Cervical injury
- Bleeding
- Uterine rupture (rare)
- Fistula formation (rare)
Postoperative Care
- Use Acetaminophen for pain relief
- Do not use vaginal tampons
- Increase rest for a few days
- Drink plenty of fluids
- Empty the bladder frequently
- Prefer sitting toilets over squatting toilets
- Avoid heavy physical activity; gradually increase activity within one week
- Abstain from intercourse for one week, and resume only after medical evaluation. If permitted, use condoms for the remainder of the pregnancy. In high-risk cases, abstinence from sexual activity and strenuous exercise may be advised until 32–34 weeks.
- Return to work after one week, if approved by the physician
- Take prescribed medications exactly as directed
- Attend weekly or biweekly follow-up visits
- Undergo transvaginal ultrasound to monitor cervical length as advised by the physician
Removal of Cerclage
- The stitch is usually removed between 36–37 weeks of pregnancy
- Removal is performed in the clinic during a simple outpatient examination
- After removal, the patient returns home and awaits the onset of labor
- Most women deliver within 2 weeks of stitch removal, though about 10% go into labor within 48 hours
Pregnancy Outcomes
The success of cerclage depends on the timing of placement. Overall, cerclage significantly reduces the risk of preterm delivery before 34 weeks and lowers the risk of pregnancy loss.