Fetal Reduction
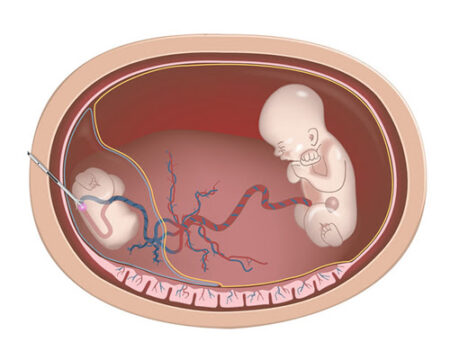
Multiple pregnancies (twins, triplets, or more) carry significantly higher risks for both the mother and the babies compared to singleton pregnancies. Ideally, careful management of IVF cycles such as controlled ovarian stimulation and limiting the number of embryos transferred can help prevent multiple pregnancies. However, when preventive strategies fail or when spontaneous multiple pregnancies occur, fetal reduction may be recommended. This procedure decreases the number of fetuses, thereby improving pregnancy outcomes and increasing the chances of survival for the remaining fetus or fetuses.
In most cases, the fetuses selected for reduction are chosen randomly based on technical factors. However, in some cases, reduction is performed selectively to terminate a fetus with confirmed genetic, chromosomal, or structural abnormalities, or severe growth restriction, diagnosed through ultrasound, CVS, or amniocentesis. This is referred to as selective termination.